COVID-19’s impact on healthcare, the economy, and everyday life will stay with us for some time. One consequence of the pandemic is the ability of patients to afford their medications. GoodRx published a recent survey on mediation affordability, with some important takeaways for pharmacy and medical leaders.
In this post, we’ll dive into the data and what it means for the healthcare ecosystem.
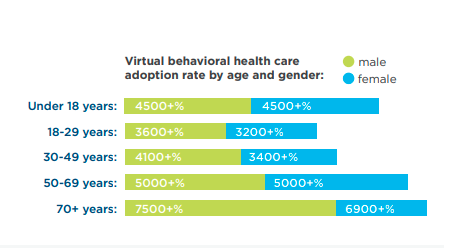
Almost 40% of Americans Struggled with Medication Affordability
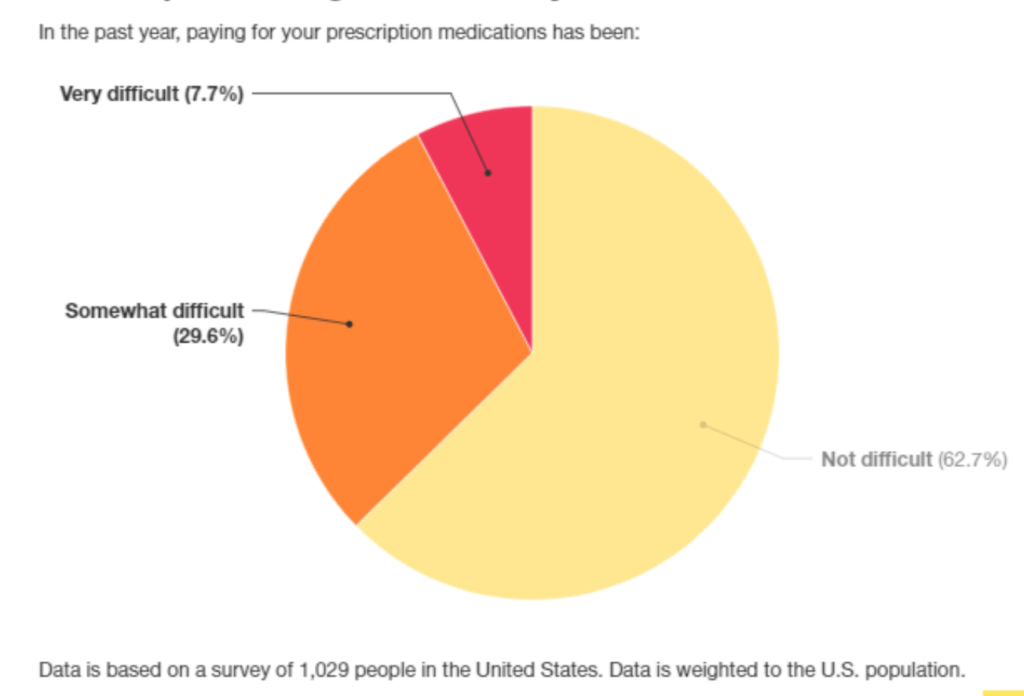
Image: GoodRx
The survey’s biggest takeaway is that a large portion had difficulty affording their prescriptions last year. The survey received answers from over 1,000 individuals that take regular drugs for chronic conditions. Almost 30% said that out-of-pocket costs for their medications went up.
In the last year, many have lost their jobs and access to health insurance. Some individuals even said increased prescriptions affected their ability to afford necessities. Choosing between food, shelter, and medication shouldn’t be a battle, but it is. That was the reality for many before the pandemic. Now more are vulnerable.
Patients Incur Debt to Pay for Meds
The survey also asked how people were paying for their prescriptions. Many tapped into their savings if they had any. Over 20% of those surveyed said they took on debt or filed bankruptcy to afford their medications.
Medication Affordability Increased Medication Nonadherence
Medication nonadherence was already a problem that costs the healthcare system substantially, with expensive hospitalization and deaths. Per the data, patients delayed getting refills, rationed, stopped taking them, and other behaviors.

Image: GoodRx
That’s dangerous and risky for patients and overburdens already maxed out hospitals. Undeniably, the pandemic made healthcare even less affordable. Nearly 24% of respondents said COVID-19 affected their ability to afford insurance.
What’s the Solution for Medication Affordability?
It’s a complex problem with lots of stakeholders. Pharma, payors, providers, pharmacies, regulators, and consumers are all at the table, having different expectations and motivations. However, people shouldn’t die or become sicker because they can’t afford their prescriptions.
Some resources are available to supplement patients. Payment assistance programs operate independently but receive funding from pharma. It can be hard to qualify for these. Medicare and Medicaid take care of many of the most vulnerable, but prescriptions can still be very costly to seniors.
There is perhaps some competition in the workings to deliver affordable medication for all. Mark Cuban is getting tin the drug business. He’s working with Cost Plus Drug Company to offer “radical transparency” to drug pricing. The company will manufacture, distribute, and market all generic drugs with a flat 15% margin. They are working to have 100 drugs available in 2021. That could reduce costs across the board and be good for pharmacies and patients.
Other opportunities for prescription affordability are discount programs like GoodRx. Their platform aggregates current prices and discounts for prescriptions by pharmacy. It lets you know which one has the best pricing and offers coupons.
Is Transparency Becoming Industry-Wide?
In these scenarios, transparency is a driving factor. Regulators are attempting to receive that same transparency from pharma and payors. The Transparency in Coverage final rule requires payers and health plans to disclose and post negotiated during prices.
For pharma, there isn’t a federal statute yet. However, multiple states have their own laws that require life sciences organizations to report their WAC (wholesale acquisition cost). Most of these programs are new, so there’s no definitive data on if disclosure will actually reduce drug prices.
Prescription Drug Costs Are Big Piece of Industry Pie
There are many drivers of increased costs in healthcare in the U.S. Prescription drugs continue to take up a large piece of the pie. A new report found U.S. drug prices are 2.56 times higher than other nations. It’s a spotlight issue that affects millions of Americans. Medication affordability was always a problem; the pandemic just expanded the impact.